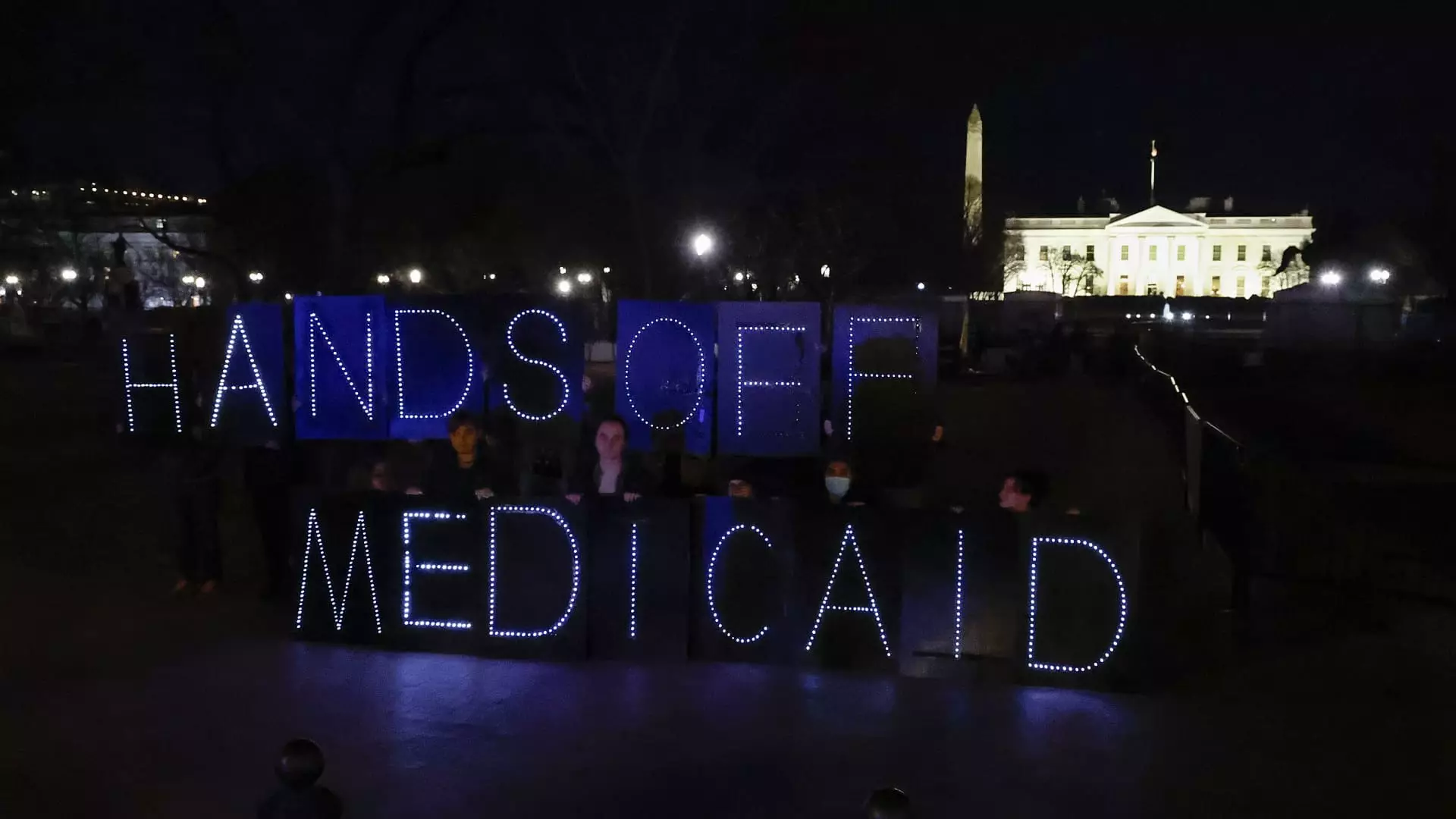
Recent revelations have surfaced from the Congressional Budget Office, illuminating a disconcerting path forward in the political arena: House Republicans may resort to drastic cuts to Medicaid in their quest for budgetary compliance. This troubling approach, embedded within a blueprint that outlines a staggering $880 billion in suggested reductions, raises profound ethical questions about the treatment of vulnerable populations. Medicaid, which is crucial for millions of low-income individuals, elderly citizens, and people with disabilities, is at the very heart of this proposed fiscal overhaul.
Lawmakers often frame these cuts in the context of financial necessity. However, within this framing lies a disquieting disregard for the human cost. As the conversation develops, it reveals an ideological cadre intent on imposing work requirements—mandating up to 80 hours of work per month to qualify for Medicaid benefits. Such policies present not just a bureaucratic hurdle, but a moral dilemma that could lead to suffering and loss for countless Americans.
Shifting Responsibility: A Flawed Narrative
The purported rationale behind work requirements—propping up a system of support by promoting personal accountability—paints a picture that neglects the nuanced realities of poverty. The widespread impression that welfare dependency can be solved through sheer willpower is rife with flaws, failing to acknowledge systemic inequalities that impede upward mobility. Farah Khan, a fellow at Brookings Metro, articulates this disconnect starkly: “When one party frames it as a moral failing to be poor because you haven’t worked hard enough, that ignores structural inequalities or systemic injustices that may have led individuals to those circumstances.”
The idea that employment equates to eligibility raises further concerns about the implications for low-income workers and their families. Data suggests that while many Americans support work requirements, only a subset of enrollees is truly amenable or able to comply with such constraints, as evidenced by a recent KFF poll revealing that 6 in 10 Americans back the concept but may lack an understanding of its potential consequences.
Historical Failures: Lessons from the Past
History has shown that states attempting to implement work requirements in Medicaid have often witnessed catastrophic outcomes. For example, Arkansas’s brief foray into such policies in 2018 resulted in one in four individuals losing coverage—around 18,000 people—within just seven months. These statistics point to a chilling reality: imposing additional conditions on essential health coverage does not incentivize employment as intended; instead, they lead to disenrollment and destabilization of lives.
Such outcomes do not merely affect the individuals directly involved; they send shockwaves through families and communities, increasing reliance on emergency services, unpaid caregivers, and ultimately failing to deliver on promised fiscal savings. Laura Harker, a senior policy analyst at the Center on Budget and Policy Priorities, sums this sentiment effectively: “Medicaid work requirements have resulted in coverage losses without incentivizing or increasing employment,” highlighting the burdensome nature of these proposals.
The Conflict of Ideologies
This perfunctory approach reflects a broader ideological clash between American conservatism and the social democratic models pervasive in many European nations. In contrast to the U.S., which often views welfare through a punitive lens, European systems tend to prioritize social safety nets as a collective responsibility to shield the most vulnerable. The misguided perception that poverty results from personal failure rather than systemic barriers continues to inform policy decisions that can devastate lives.
In view of conservative viewpoints, they contend that offering support without work incentives creates a dependency culture. However, this argument lacks empirical backing, further emphasized by research from the American Enterprise Institute noting that many working-age Medicaid recipients do not log enough hours to meet a rigid 80-hour requirement. This points to an all-too-important need for an empathy-driven approach to social welfare that marries accountability with compassion, acknowledging the everyday struggles of those caught in the crossfire of economic realities.
The Unsustainable System: Administrative Barriers and Human Costs
The introduction of work requirements in Medicaid is not merely a political maneuver; it risks creating an unsustainable and punitive system. The complexities of compliance—replete with bureaucratic red tape—present formidable challenges for both working individuals and those who are temporarily non-employed due to caretaking roles, disabilities, or illness. The end result is a cycle of disenrollment that can inadvertently push people further into economic despair.
It’s crucial to recognize that the majority of Medicaid enrollees—about 90%—are already engaged in the workforce or meet exemption criteria. Thus, revamping the program with work requirements could paradoxically exacerbate poverty and health insecurity. The path forward requires a reevaluation of how we perceive and structure safety nets, envisioning a more forgiving paradigm that humanizes rather than demonizes those in need.